Prevent constant embarrassment from skin rashes, stasis ulcers, and unsightly skin color change from venous insufficiency. Knowing how this disorder manifests and persists will help you take proactive measures against it.

yourfootpalace.com gathered the following information about what venous insufficiency is, its causes, the accompanying symptoms, how it is diagnosed, what you can do to treat venous insufficiency, and prevention strategies.
What Is Chronic Venous Insufficiency?
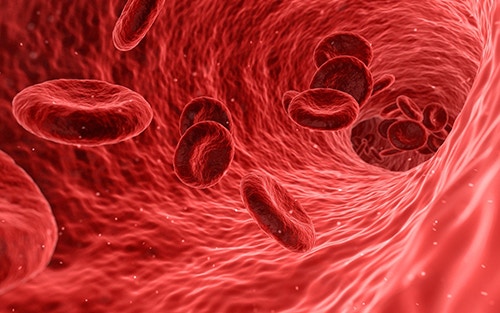
Chronic Venous Insufficiency (CVI) happens when your leg veins stop functioning properly and stop directing blood flow back to your heart. Normally, valves in your veins ensure that blood flows toward your heart. However, when these valves malfunction, blood is permitted to flow backward. This can cause blood to collect or pool in your legs.
Note: In the medical field, the acronym “CVI” is also derived from Cortical Visual Impairment and/or Cerebral Visual Impairment.
What Causes Chronic Venous Insufficiency?
You are more likely to develop this condition if you:
- Are overweight or obese
- Are pregnant
- Have a family history of a contributing condition or ailment
- Suffered damage to your leg due to injury, surgery, or past blood clots
- Have or have had pelvic tumors
- Have vascular malformations
Other potential causes of chronic venous insufficiency include:
- Aging
- Reduced mobility
- High blood pressure in leg veins over time, from sitting or standing for long periods
- Lack of activity or exercise
- Smoking (at any quantity or frequency)
- A blood clot in a deep vein, often in the calf or thigh (deep vein thrombosis – DVT)
- Vein swelling and/or inflammation close to the skin, frequently in the legs (phlebitis)
- Sometimes CVI can occur for unknown reasons
Note: Chronic venous insufficiency resulting from DVT is also referred to as post-thrombotic syndrome. Approximately 30 percent of people diagnosed with DVT will likely develop CVI within 10 years after diagnosis.
Veins are responsible for returning blood to the heart from all the body’s organs and limbs. To get to the heart, blood needs to flow upward from veins in the legs. Your calf and foot muscles need to contract with each step, which applies pressure to the veins and pushes blood upward. To keep blood flowing back to the heart and not back down, the veins contain one-way valves.
CVI develops when these one-way valves become defective or damaged, allowing blood to reverse course. When veins and their valves are debilitated to the point where it becomes difficult for blood to flow back to the heart, blood pressure in the veins stays elevated for long periods, leading to chronic venous insufficiency.
What are the Symptoms of Chronic Venous Insufficiency?

The seriousness of CVI and the complexities of eventual treatment will increase as the affliction progresses. This is why it is imperative to see your doctor if you have any or a combination of the following CVI symptoms:
- Leathery skin on the legs (often accompanied by hair loss in the area)
- Dry, flaking, and/or itching skin on the legs or feet
- Stasis ulcers or venous stasis ulcers caused by fluid build-up in the skin
- Swelling in lower legs and ankles, primarily after extended periods of standing or sitting
- Aching or tiredness in the legs
- Newly developed varicose veins
Note: Untreated CVI will increase pressure and swelling until the tiniest blood vessels in the legs (capillaries) rupture. When these blood vessels rupture, the overlying skin turns a reddish-brown color and becomes very sensitive to being broken when bumped or scratched.
Burst capillaries can cause local tissue inflammation and internal tissue damage. When left untreated or ignored, this can lead to ulcers, open sores on the skin surface. These venous stasis ulcers may be difficult to heal and can develop infections. If this type of infection is not controlled, it can quickly spread to surrounding tissue. This condition is known as cellulitis.
CVI is often associated with varicose veins, which are twisted, enlarged veins close to the skin’s surface. They can occur almost anywhere but most commonly occur in the legs.

Tip: These problems will not go away if you procrastinate seeking help. The earlier it is diagnosed and treated, the better your chances are at preventing more severe complications.
How Is Chronic Venous Insufficiency Diagnosed?
Your primary care physician will likely need to do a complete physical examination and get your full medical history to accurately deduce if you do, in fact, have venous insufficiency.
Imaging tests may be used to locate the source of the condition. These tests may include a venogram or a duplex ultrasound:
Venogram
- Your doctor will put an intravenous (IV) contrast dye into your veins.
- The contrast dye causes blood vessels to appear opaque on the X-ray image so they may be seen.
- This dye will give your doctor a clearer X-ray picture of your blood vessels.
Duplex Ultrasound
- A vascular or duplex ultrasound may be used to test the speed and direction of blood flow in the veins.
- A technician places gel on the skin and then presses a hand-held device (transducer) against the area.
- The transducer uses sound waves that bounce back to a computer which produces images of blood flow.
Note: Correctly diagnosing your CVI is crucial for your doctor when developing an effective and personalized treatment plan.
How Is Chronic Venous Insufficiency Treated?
The type and the duration of CVI treatment will depend on multiple factors, including the reason for the condition combined with your health status and history. Other factors your doctor will consider are:
- Your symptoms
- Your age
- The severity of your condition
- How well you can tolerate medications or procedures
The most common venous insufficiency treatment is prescribing compression stockings. These special elastic stockings apply pressure at the ankle and lower leg. They help improve blood flow and can dramatically reduce leg swelling.

Compression stockings come in a range of prescription strengths and different lengths. Your doctor will help you determine the best compression stocking option for your treatment.
Treatment for venous insufficiency can include multiple strategies like Improving blood flow:
- Cease all tobacco usage
- Keep your legs elevated (above your waistline) whenever possible
- Wear compression stockings
- Keep your legs uncrossed when seated
- Exercise regularly (walk when possible)
- Have regular massages and spa days
- Moisturize skin to prevent cracking
Note: Massage therapies such as vascular and lymphatic drainage massages that aim to increase circulation and improve tissue nutrition are beneficial to patients with varicose veins and chronic venous insufficiency
Medications
There are a number of medications that may help those who have this condition. These include:
- Diuretics – Medications that draw fluid from your body that is excreted through the kidneys
- Anticoagulants – These are medications that thin the blood
- Pentoxifylline (Trental) – This medication helps improve blood flow
Surgery
Sometimes more severe cases of CVI require surgery. Your doctor may suggest one of the following:
- Surgical repair of veins or valves
- Removing (stripping) damaged veins
- Minimally invasive endoscopic surgery – The surgeon inserts a tube with a camera on it to help see and tie off varicose veins.
- Vein bypass – A healthy vein is transplanted from another location in your body. This procedure is generally used only in the upper thigh and only as a last resort for very severe cases.
- Laser surgery – A relatively new treatment using lasers to either fade or close the damaged vein(s).

Ambulatory Phlebectomy
This is an outpatient procedure (you won’t have to spend the night in the hospital). It involves your doctor numbing specific locations on your leg, making small pricks, and removing smaller varicose veins.
Sclerotherapy
This treatment is usually reserved for advanced venous insufficiency.
In sclerotherapy, a chemical is injected into a damaged vein so it can no longer carry blood. Blood returns to the heart through other veins, and the damaged vein is eventually absorbed by the body.
Catheter Procedures
In more severe cases, your doctor can use a catheter procedure for larger veins. A catheter is inserted into the vein, the end of the catheter is heated, then the catheter is removed. The heat causes the vein to close and seal.
Can Chronic Venous Insufficiency Be Prevented?
You can alter your lifestyle to reduce the risk of developing CVI, consider the following:
- Eat a healthy balanced diet
- Quit smoking (cease all consumption/use of tobacco-based or nicotine products)
- Exercise regularly (walking is highly recommended)
- Avoid wearing restrictive clothing such as tight girdles or belts
- Lose weight if you are overweight or obese
- Avoid prolonged sitting or standing
- Don’t cross your legs when seated
Tip: Ask your primary care physician for referrals to a physical trainer and a nutritionist that can help structure these activities.
Chronic Venous Insufficiency
In this article, you discovered information about venous insufficiency, what causes it, accompanying symptoms, how it is diagnosed, what treatments can be used, and what you can do to reduce your risk of developing it.
Knowing how to recognize and deal with blood circulation problems will help you get the assistance you need before those problems become catastrophic or life-threatening.
Ignoring signs and symptoms of venous insufficiency can lead to severe discomfort, pain, stasis ulcers, and other complications that can land you in the hospital or worse.
Sources:
hopkinsmedicine.org/health/conditions-and-diseases/chronic-venous-insufficiency
cedars-sinai.org/health-library/diseases-and-conditions/c/chronic-venous-insufficiency.html
my.clevelandclinic.org/health/diseases/16872-chronic-venous-insufficiency-cvi
medlineplus.gov/ency/article/000203.htm
(706) 521-5290
(678) 963-5958








