Prevent leg pain and swelling from leaving you immobilized and vulnerable to developing severe life-threatening conditions. Knowing what to do when uncomfortable or debilitating leg conditions develop can ultimately save your life.

yourfootpalace.com gathered the following information about tightening and swelling sensations in the legs, some potential causes, how to treat this condition, and how to prevent it.
Intermittent Claudication
Description – Intermittent claudication is a tight, aching, or squeezing pain in the calf, foot, thigh, or buttock that occurs during exercise, like walking up a hill, steep trail, or a flight of stairs. This pain is a symptom of peripheral neuropathy or peripheral arterial disease (PAD).
Symptoms – People with intermittent claudication commonly describe their leg pain as a deep, gradually worsening tightening – until they rest. The lower legs may cramp up or feel weak.
If you experience pain while at rest, without exercising, this may indicate an advanced arterial blockage. If appropriate treatment is not started immediately, tissue death can rapidly occur.
The pain is often noticed at night and is relieved by hanging the affected leg off of your bed or couch. The pain also may improve with walking since gravity helps blood reach the foot. As this condition worsens, the accompanying pain may interrupt sleep, resulting in a lack of appetite and make the affected leg sensitive to the touch.
Treatment – Treatments may include increasing blood and oxygen delivery to muscles as their oxygen requirements increase and scheduling more time for massage therapy and/or spa treatments. Read our blog for more information on how massage can relieve your peripheral neuropathy pain.
Myocardial Ischemia
Description – Myocardial ischemia occurs when blood flow to the heart muscle (myocardium) is obstructed by a partial or complete blockage of a coronary artery by a buildup of plaques (atherosclerosis). If the plaques rupture, you can have a heart attack (myocardial infarction).
Causes and Symptoms – Ischemia can have causes that aren’t due to underlying disease. Examples include extreme exercise, cold exposure, or tourniquet.
Seek a doctor immediately if you:
- Get sudden, severe belly pain
- Feel prolonged or severe chest pain
- Have numbness or weakness on one side of the body
- Slur your speech
Make an appointment to see a doctor if you:
- Get chest or leg pain after exercise
- Have bowel movements more or less frequently
- Feel abdominal pain after eating
Note: Seek emergency medical help by dialing 9-1-1 if you have severe chest pain or chest pain that doesn’t go away.
Treatment – Treatment for myocardial ischemia focuses on improving blood flow to the heart muscle. Treatment may include:
- Medications
- Angioplasty (a procedure to open blocked arteries)
- Bypass surgery
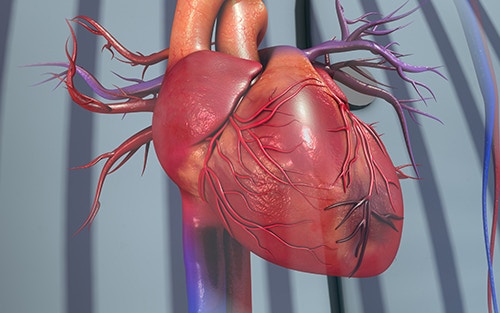
Note: Making heart-healthy lifestyle choices is important in treating and preventing myocardial ischemia.
Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE)
Description – Deep vein thrombosis (DVT) is a medical condition that occurs when a blood clot forms in a deep vein. These clots usually develop in the lower leg, thigh, or pelvis, but they can also occur in the arm. A pulmonary embolism (PE) usually happens when a deep vein thrombosis (DVT) travels to your lungs and obstructs a blood vessel. This results in low oxygen levels in your blood. If left untreated, it can damage the lung and other organs, potentially causing heart failure.
Symptoms – About half of people with DVT have no symptoms at all. However, the following are the most common symptoms of DVT that occur in the affected part of the body:
- Swelling
- Pain
- Tenderness
- Skin Redness
If you have any of these symptoms, you should see your doctor as soon as possible.
Risk Factors for DVT
Almost anyone can have a DVT. However, certain factors can increase the chance of having this condition. The chance increases even more for someone who has more than one of these factors at the same time.
The following are factors that increase the risk of developing DVT:
Injury to a vein, often caused by:
- Fractures
- Severe muscle injury
- Major surgery (particularly involving the abdomen, pelvis, hip, or legs)
Slow blood flow, often caused by:
- Confinement to bed (e.g., due to a medical condition or after surgery)
- Limited movement (e.g., a cast on a leg to help heal an injured bone)
- Sitting for a long time, especially with crossed legs
- Paralysis.
Increased estrogen, often caused by:
- Birth control pills
- Hormone replacement therapy, sometimes used after menopause
- Pregnancy, for up to 3 months after giving birth

Certain chronic medical illnesses, such as:
- Heart disease
- Lung disease
- Cancer and its treatment
- Inflammatory bowel disease (Crohn’s disease or ulcerative colitis)
Other factors that increase the risk of DVT include:
- Previous DVT or PE
- Family history of DVT or PE
- Age (risk increases as age increases)
- Smoking (at any quantity or frequency)
- Obesity
- A catheter located in a central vein
- Inherited clotting disorders
Preventing DVT and PE
The following tips can help prevent DVT:
Move around as soon as possible after having been confined to bed, such as after surgery, illness, or injury.
If you’re considered at risk for DVT, talk to your doctor about:
- Wearing graduated compression stockings (sometimes called “medical compression stockings”)
- Medication (anticoagulants) to prevent DVT
When sitting for long periods, such as when traveling for more than four hours:
- Get up and walk around every 2 to 3 hours
- Take advantage of frequent rest stops
Exercise your legs and protect them while sitting by:
- Raising and lowering your heels while keeping your toes on the floor
- Raising and lowering your toes while keeping your heels on the floor
- Maintaining good posture throughout long trips
- Tightening and releasing your leg muscles
- Wearing loose-fitting clothes
You can significantly reduce your risk of DVT by maintaining a healthy weight, avoiding a sedentary lifestyle, and abiding by your doctor’s recommendations based on your risk factors.
Why Do My Legs Hurt?
Take note that in the conditions mentioned earlier, each, in one way or another, results in or from restricted/obstructed blood flow and severely reduced oxygen levels (Hypoxemia) in the blood.
What Are the Complications of Hypoxemia?
If your blood does not carry sufficient oxygen, it cannot deliver enough oxygen to your organs and tissues. This condition can be fatal when severe in the short term and can affect your heart or brain if it persists over a long period.
How To Prevent Hypoxemia
The following may be recommended for you to increase oxygen levels in your blood:
- Drinking plenty of water
- Quitting smoking
- Deep breathing exercises
- Mild exercises such as walking or yoga
- Eating a healthy diet
What is Chronic Venous Insufficiency (CVI)
Chronic Venous Insufficiency happens when your leg veins stop functioning properly and stop directing blood flow back to your heart. Usually, valves in your veins ensure that blood flows toward your heart. However, when these valves malfunction, blood is permitted to flow backward. This may lead to blood collecting or pooling in your legs.
You are more at risk of developing this condition if you:
- Smoking (at any quantity or frequency)
- Are overweight or obese
- Are pregnant
- Suffered damage to your leg due to injury, surgery, or past blood clots
- Have high blood pressure in leg veins over time, from sitting or standing for long periods
- Lack of activity or exercise
Read more about Chronic Venous Insufficiency by visiting yourfootpalace.com/chronic-venous-insufficiency-causes-symptoms-treatment
Swollen and Tight legs
In this article, you discovered crucial information about the causes, symptoms, treatment, and prevention of tightening and swelling legs.
Taking swift action to identify and treat conditions contributing to your leg pain can help you quickly regain your mobility and confidence.
Ignoring the signs your body manifests when something is wrong can end with fatal results. Nearly every physical and mental condition is treated more efficiently, with higher success rates.
Sources:
uofmhealth.org/health-library/ue4732
mayoclinic.org/diseases-conditions/myocardial-ischemia/symptoms-causes/syc-20375417
cdc.gov/ncbddd/dvt/facts.html
(706) 521-5290
(678) 963-5958