When your adrenal glands fail to produce essential hormones, the consequences can be life-threatening without proper recognition and treatment. Adrenal insufficiency is a rare but serious endocrine disorder that affects how your body responds to stress, maintains blood pressure, and regulates vital metabolic processes.
This comprehensive guide will walk you through everything you need to know about adrenal insufficiency, from understanding the different types to recognizing emergency symptoms and managing daily life with this condition. Whether you’re newly diagnosed, caring for someone with adrenal dysfunction, or simply seeking reliable medical information, this article provides the essential knowledge you need.
What is Adrenal Insufficiency?
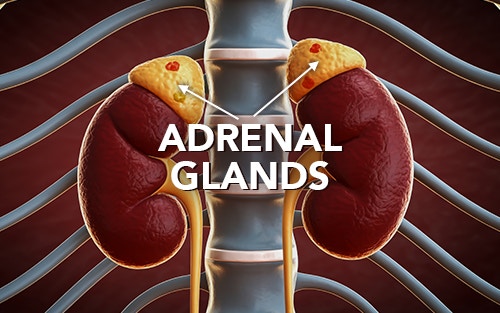
Adrenal insufficiency occurs when the adrenal glands, two small triangular organs located above your kidneys, fail to produce adequate amounts of essential steroid hormones. These hormones, particularly cortisol and aldosterone, play crucial roles in maintaining your body’s normal functions.
The adrenal cortex, which forms the outer layer of each adrenal gland, is responsible for producing these life-sustaining hormones. Cortisol helps your body respond to physical stress, regulates blood sugar levels, and modulates your immune system. Aldosterone controls blood pressure by managing sodium and potassium balance in your body.
When the adrenal cortex cannot produce enough cortisol, your body loses its ability to handle stress effectively. This can lead to a cascade of potentially life-threatening complications, especially during periods of illness, injury, or emotional stress. The condition affects approximately 93-140 people per million in the general population, making it a rare condition that requires specialized medical care.
Without proper hormone replacement therapy, adrenal insufficiency can progress to acute adrenal failure, also known as adrenal crisis – a medical emergency that can be fatal if not treated immediately.
Types of Adrenal Insufficiency
Understanding the various types of adrenal insufficiency is crucial for accurate diagnosis and effective treatment. The classification depends on where the problem originates in the hormone production pathway.
Primary Adrenal Insufficiency (Addison’s Disease)
Primary adrenal insufficiency, also known as Addison’s disease, results from direct damage to the adrenal glands themselves. This is the most severe form because it affects both cortisol and aldosterone production.
The most common cause is autoimmune Addison’s disease, where the immune system mistakenly attacks the healthy tissues of the adrenal cortex. This autoimmune condition accounts for disproportionately large number of the cases in developed countries. The immune system attacks the cells responsible for hormone production, gradually destroying the gland’s ability to function.
Other causes of primary adrenal insufficiency include:
- Infectious diseases such as tuberculosis, HIV, and fungal infections
- Bilateral adrenal hemorrhage during severe illness or blood-clotting disorders
- Cancer cells that have spread to both adrenal glands
- Genetic conditions like congenital adrenal hyperplasia
- Surgical removal of both adrenal glands
Secondary Adrenal Insufficiency
Secondary adrenal insufficiency is referred to as such because it originates from problems with the pituitary gland. The pituitary gland makes adrenocorticotropic hormone (ACTH), which signals the adrenal glands to produce cortisol.
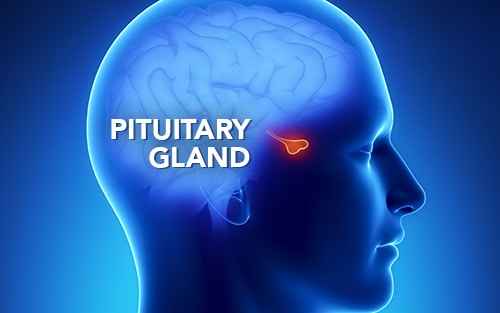
When the pituitary gland doesn’t produce enough ACTH, the adrenal glands receive insufficient stimulation to make adequate cortisol. However, aldosterone production typically remains normal because it’s primarily controlled by the renin-angiotensin system rather than ACTH.
Common causes include:
- Pituitary tumors or pituitary adenoma
- Surgical removal of pituitary tissue
- Radiation therapy to the head
- Traumatic brain injury affecting the pituitary gland
- Sudden discontinuation of long-term glucocorticoid treatment
Tertiary Adrenal Insufficiency
Tertiary adrenal insufficiency results from hypothalamic dysfunction, where the brain fails to produce enough corticotropin-releasing hormone (CRH). This is most commonly seen after prolonged glucocorticoid treatment that suppresses the entire hypothalamic-pituitary-adrenal axis.
When patients stop taking steroids suddenly after extended use, their natural hormone production system may not restart immediately, leading to temporary but potentially dangerous hormone deficiency.
Causes and Risk Factors
The underlying causes of adrenal insufficiency vary significantly depending on the type and the patient’s demographics. Understanding these risk factors helps healthcare providers maintain a proper clinical suspicion for diagnosis.
Autoimmune Causes
Autoimmune Addison’s disease represents the leading cause of primary adrenal insufficiency in developed nations. This autoimmune disease often occurs alongside other autoimmune disorders, forming what the endocrine society recognizes as autoimmune polyendocrine syndromes.
Patients with autoimmune Addison’s disease frequently have other conditions such as:
- Type 1 diabetes mellitus
- Autoimmune thyroid disease
- Premature ovarian failure
- Chronic autoimmune hepatitis
The National Institute of diabetes and Digestive and Kidney Diseases reports that these autoimmune disorders tend to cluster in families, suggesting genetic predisposition plays a significant role.
Infectious Causes
While less common in developed countries, infectious causes remain significant globally, particularly in developing countries where tuberculosis is endemic. The infection can directly invade and destroy adrenal tissue, leading to permanent hormone deficiency.
HIV infection increases the risk of various opportunistic infections that can affect the adrenal glands, including cytomegalovirus and histoplasmosis. These fungal infections can cause bilateral adrenal destruction in immunocompromised patients.
Medication-Related Causes
One of the most preventable causes of adrenal insufficiency is the inappropriate discontinuation of long-term steroid therapy. When patients receive glucocorticoid treatment for extended periods, their natural hormone production shuts down.
Healthcare providers must carefully taper steroid medications to allow the hypothalamic-pituitary-adrenal axis to recover gradually. Abrupt cessation can precipitate acute adrenal crisis within days or weeks.
Genetic and Congenital Factors
Several genetic conditions can cause adrenal insufficiency, particularly in children and young adults. Congenital adrenal hyperplasia represents a group of inherited disorders affecting hormone synthesis enzymes.
Signs and Symptoms
Recognizing the signs and symptoms of adrenal insufficiency can be challenging because they often develop gradually and mimic other common medical conditions. However, understanding both the chronic presentation and acute emergency symptoms is essential for proper diagnosis and treatment.
Chronic Symptoms
The most common symptoms of adrenal insufficiency develop slowly over months or years as hormone deficiency gradually worsens. These chronic manifestations often lead to delayed diagnosis because they’re nonspecific.

Extreme Fatigue and Muscle Weakness
Persistent, overwhelming fatigue that doesn’t improve with rest is one of the hallmark symptoms. Patients often describe feeling completely drained of energy, even after minimal physical activity. This fatigue differs from normal tiredness and significantly impacts daily functioning.
Muscle weakness typically affects the entire body but may be more noticeable in the arms and legs. Simple tasks, such as climbing stairs or lifting objects, become increasingly difficult.
Weight Loss and Appetite Changes
Unintentional weight loss occurs in most patients, often accompanied by decreased appetite and nausea. The weight loss can be substantial, sometimes 10-15 pounds or more over several months.
Salt craving is particularly characteristic of primary adrenal insufficiency, as patients unconsciously seek to replace lost sodium. This craving can be intense and persistent.
Gastrointestinal Symptoms
Abdominal pain, nausea, and vomiting are frequent complaints that may initially suggest gastrointestinal disorders. These symptoms often worsen during periods of stress or illness.
Diarrhea and general digestive upset can contribute to dehydration and electrolyte imbalances, particularly dangerous in patients who already have compromised hormone regulation.
Cardiovascular Symptoms
Low blood pressure is extremely common, particularly orthostatic hypotension, where blood pressure drops significantly upon standing. This can cause dizziness, lightheadedness, and fainting episodes.
Patients may notice their heart racing when they stand up or during mild physical activity as their cardiovascular system struggles to maintain adequate circulation.
Distinctive Skin Changes
In primary adrenal insufficiency specifically, hyperpigmentation or darkened skin develops in sun-exposed areas, skin creases, and mucous membranes. This occurs because elevated ACTH levels stimulate melanin production.
The darkening is most noticeable on the knuckles, elbows, knees, and inside the mouth. This symptom doesn’t occur in secondary or tertiary forms where ACTH levels are low.
Neuropsychiatric Effects
Depression, irritability, and cognitive difficulties are common but often overlooked symptoms. Patients may experience mood swings, difficulty concentrating, and memory problems.
These mental health effects can significantly impact quality of life and may be mistakenly attributed to stress or other psychological conditions.
Gender-Specific Symptoms
Women with adrenal insufficiency often experience menstrual irregularities or complete loss of periods (amenorrhea). Decreased body hair growth, particularly in the pubic and underarm areas, may also occur due to reduced androgen production.
Men may notice decreased body hair and reduced muscle mass, along with potential fertility issues.
Adrenal Crisis (Emergency Symptoms)
Adrenal crisis represents the most serious complication of adrenal insufficiency and constitutes a true medical emergency. This acute adrenal failure can develop rapidly and requires immediate emergency treatment.

Severe Cardiovascular Collapse
The most dangerous aspect of adrenal crisis is severe hypotension that can progress to shock. Blood pressure may drop to critically low levels, causing inadequate blood flow to vital organs.
Heart rhythm abnormalities can occur due to dangerous electrolyte imbalances, particularly elevated potassium levels that can affect cardiac function.
Extreme Dehydration
Patients in adrenal crisis become severely dehydrated due to the loss of aldosterone’s effects on kidney function. This dehydration compounds the low blood pressure and can lead to kidney failure.
High Fever and Altered Mental Status
Body temperature may spike to dangerous levels, often exceeding 104°F (40°C). Along with fever, patients may become confused, delirious, or lose consciousness entirely.
Severe Gastrointestinal Symptoms
Intense nausea and vomiting prevent patients from keeping down fluids or medications, worsening dehydration. Severe abdominal pain may mimic surgical emergencies.
Life-Threatening Electrolyte Imbalances
Blood sodium levels drop dangerously low (hyponatremia) while potassium levels rise to toxic ranges (hyperkalemia). These imbalances can cause seizures, cardiac arrest, and coma.
Hypoglycemia
Blood sugar levels may drop precipitously, particularly in children, causing weakness, confusion, and potentially coma.
The mortality rate for untreated adrenal crisis approaches 10%, but with prompt recognition and appropriate emergency treatment, most patients recover fully. Any patient with known adrenal insufficiency who develops severe illness should receive immediate medical attention and stress-dose steroids.
Diagnosis of Adrenal Insufficiency
Diagnosing adrenal insufficiency requires a systematic approach that combines clinical suspicion, laboratory testing, and, in some cases, imaging studies. The diagnostic process aims to confirm hormone deficiency and determine whether the problem lies in the adrenal glands themselves or in the pituitary-hypothalamic control system.
Initial Laboratory Testing

Morning Cortisol Levels
The diagnostic workup typically begins with measuring plasma cortisol levels in the early morning when they should be at their highest. A morning cortisol level below a certain threshold suggests adrenal insufficiency. There is also an indeterminate range where further testing and evaluation is necessary.
ACTH Stimulation Test
The short ACTH stimulation test, also called the cosyntropin test, is considered the gold standard for diagnosing adrenal insufficiency. This test measures how well the adrenal glands respond to synthetic ACTH stimulation.
During the test, patients receive an injection of synthetic ACTH, and blood samples are drawn before and 30-60 minutes after the injection to measure cortisol response. A normal response is characterized by a significant rise in cortisol levels, whereas a blunted or absent response indicates adrenal insufficiency.
This test can differentiate between primary and secondary forms:
- In primary adrenal insufficiency, the cortisol response is severely impaired
- In secondary adrenal insufficiency, the response may be normal or only mildly impaired, depending on the duration of ACTH deficiency.
Additional Diagnostic Tests
ACTH Levels
Measuring baseline ACTH levels helps distinguish between primary and secondary causes:
- Primary adrenal insufficiency shows markedly elevated ACTH
- Secondary and tertiary forms typically have low or inappropriately normal ACTH levels
Electrolyte Panels
Blood tests frequently reveal characteristic electrolyte abnormalities:
- Hyponatremia (low sodium) occurs in about 90% of patients
- Hyperkalemia (elevated potassium) is common in primary adrenal insufficiency
- Hypoglycemia may be present, particularly in children
Plasma Renin Activity
Elevated plasma renin activity combined with low aldosterone levels confirms mineralocorticoid deficiency in primary adrenal insufficiency. This test helps determine whether patients need mineralocorticoid replacement therapy.
Specialized Testing
Autoantibody Testing
Testing for 21-hydroxylase autoantibodies can confirm autoimmune Addison’s disease. These antibodies are present in about 95% of patients with autoimmune adrenal destruction.
Other autoantibodies may be tested if polyglandular autoimmune syndromes are suspected, including thyroid peroxidase antibodies and islet cell antibodies.
Imaging Studies

Computed tomography or MRI scans of the adrenal glands may be indicated when:
- The cause of primary adrenal insufficiency is unclear
- Infectious causes are suspected
- Adrenal hemorrhage or tumors are possible
- The patient has rapid-onset symptoms
Imaging can reveal:
- Adrenal atrophy in autoimmune disease
- Calcification suggesting previous tuberculosis infection
- Bilateral enlargement in infiltrative diseases
- Evidence of hemorrhage or metastatic disease
Additional Pituitary Testing
When secondary adrenal insufficiency is suspected, comprehensive pituitary function testing may be necessary to confirm the diagnosis. This includes measuring other pituitary hormones such as growth hormone, thyroid-stimulating hormone, and reproductive hormones.
MRI of the pituitary gland can identify tumors, inflammation, or structural abnormalities that might explain secondary adrenal insufficiency.
Treatment and Management
Effective treatment of adrenal insufficiency requires lifelong hormone replacement therapy, careful monitoring, and patient education about managing stress situations. The treatment approach varies depending on the type of adrenal insufficiency and the specific hormones that need to be replaced.
Hormone Replacement Therapy
Glucocorticoid Replacement
All patients with adrenal insufficiency require glucocorticoid replacement to replace cortisol. The most commonly used medications include:
- Hydrocortisone: The preferred choice because its structure most closely matches natural cortisol. Typically doses are divided into several doses to mimic the body’s natural rhythm.
- Prednisone or Prednisolone: Alternative options that may be used when hydrocortisone is not available or well-tolerated.
The dosing schedule aims to replicate normal cortisol patterns, with higher doses in the morning and lower doses in the evening. Many patients take two-thirds of their daily dose upon waking and one-third in the late afternoon.
Mineralocorticoid Replacement
Patients with primary adrenal insufficiency also need mineralocorticoid replacement because their adrenal glands cannot produce aldosterone. Fludrocortisone is a common treatment, typically dosed daily.
Secondary and tertiary adrenal insufficiency usually don’t require mineralocorticoid replacement because the adrenal glands can still produce aldosterone in response to the renin-angiotensin system.
Androgen Replacement
Some patients, particularly women with primary adrenal insufficiency, may benefit from androgen replacement with dehydroepiandrosterone (DHEA). This is especially considered when patients experience persistent fatigue, decreased well-being, or reduced libido despite optimal glucocorticoid and mineralocorticoid replacement.

Stress-Dose Management
One of the most critical aspects of treatment involves teaching patients how to adjust their medication during periods of physical stress, illness, or medical procedures. This concept, known as “stress dosing,” prevents adrenal crisis during times when the body would typically increase cortisol production.
Sick Day Rules
Patients learn to recognize situations requiring increased glucocorticoid doses:
- Minor stress (mild cold, dental work): Double the daily dose
- Moderate stress (fever, significant illness, minor surgery): Triple the daily dose
- Major stress (severe illness, major surgery, trauma): May require higher hydrocortisone equivalents
These adjustments continue until the stressful situation resolves, then patients gradually return to their baseline dose.
Injectable Emergency Medication
All patients should carry emergency hydrocortisone injections for situations where they cannot take oral medication due to vomiting or altered consciousness. Patients and family members receive training on proper injection techniques.
Emergency Treatment
Adrenal crisis requires immediate emergency treatment that cannot wait for laboratory confirmation of the diagnosis. The treatment protocol includes:
Immediate Interventions
- High-dose intravenous hydrocortisone: Followed by continuous infusion or repeated doses
- Aggressive fluid resuscitation: Rapid administration of normal saline to correct dehydration and hypotension
- Electrolyte correction: Monitoring and correcting sodium and potassium imbalances
- Blood glucose management: Treating hypoglycemia with intravenous dextrose
Supportive Care
- Identifying and treating precipitating causes, such as infections
- Monitoring vital signs and cardiac rhythm
- Managing fever and pain
- Providing intensive care monitoring for severe cases
Long-term Monitoring
Regular follow-up care ensures optimal hormone replacement and early detection of complications. Monitoring typically includes:
Clinical Assessment
- Evaluation of symptoms, energy levels, and quality of life
- Blood pressure monitoring, particularly for signs of over- or under-replacement
- Weight and physical examination
- Assessment of medication adherence and stress-dosing understanding
Laboratory Monitoring
- Plasma renin activity to assess mineralocorticoid dose adequacy
- Electrolyte levels to ensure proper sodium and potassium balance
- Bone density screening due to increased fracture risk with long-term steroid use
Patient Education Review
Regular reinforcement of stress-dosing protocols, emergency procedures, and recognition of crisis symptoms ensures patients can manage their condition safely.
Living with Adrenal Insufficiency
Successfully managing adrenal insufficiency extends far beyond taking daily medications. Patients must develop comprehensive strategies to maintain their health, prevent emergencies, and preserve their quality of life while living with this chronic condition.
Daily Management Strategies
Medication Adherence
Consistent medication timing is crucial for maintaining stable hormone levels. Patients should:
- Take morning doses immediately upon waking to replicate the natural cortisol rhythm
- Use pill organizers and smartphone reminders to ensure doses aren’t missed
- Keep backup medications in multiple locations (home, work, car, travel bag)
- Never run out of medication by refilling prescriptions early
Dietary Considerations
While no specific diet is required, certain nutritional principles support optimal health:
- Adequate sodium intake: Particularly important for patients with primary adrenal insufficiency who need extra salt
- Calcium and vitamin D supplementation: Essential for bone health due to long-term steroid use
- Regular meals: Helps maintain stable blood sugar levels
- Increased fluid intake: Especially during hot weather or exercise
Exercise and Physical Activity
Regular exercise benefits overall health but requires careful planning:
- Start slowly and gradually increase intensity
- Monitor for unusual fatigue or symptoms during activity
- Consider increasing medication doses for prolonged or intense exercise
- Stay well-hydrated and maintain electrolyte balance
Emergency Preparedness
Medical Alert Identification
All patients should wear medical alert bracelets or carry cards indicating:
- Diagnosis of adrenal insufficiency
- Current medications and doses
- Emergency contact information
- Instructions for emergency steroid administration

Emergency Kit Preparation
Patients should always carry an emergency kit containing:
- Injectable hydrocortisone with syringes
- Extra oral medications for several days
- Written instructions for emergency procedures
- Emergency contact numbers
- Copy of recent laboratory results
Travel Considerations
Traveling requires additional preparation:
- Carry medications in carry-on luggage with prescriptions
- Bring extra medication for unexpected delays
- Adjust for time zone changes gradually
- Research medical facilities at the destination
- Consider travel insurance covering pre-existing conditions
Family and Caregiver Education
Crisis Recognition Training
Family members and close friends should learn to recognize adrenal crisis symptoms and know how to:
- Administer emergency injections
- Contact emergency medical services
- Provide a clear medical history to healthcare providers
- Support the patient during recovery
Workplace Accommodations
Patients may benefit from workplace accommodations such as:
- Flexible scheduling for medical appointments
- Access to refrigeration for medications
- Understanding supervisors regarding sudden illness
- Reduced exposure to workplace stressors when possible
Psychological and Social Support
Mental Health Considerations
Living with a chronic, potentially life-threatening condition can affect mental health:
- Regular counseling or therapy may help with adjustment
- Support groups connect patients with others facing similar challenges
- Depression and anxiety should be addressed promptly
- Stress management techniques support overall well-being
Relationship Impact
Adrenal insufficiency can affect personal relationships:
- Open communication about the condition helps partners understand limitations
- Planning social activities around medication schedules and energy levels
- Educating friends and family reduces anxiety and improves support
Quality of Life Optimization
Energy Management
Patients often need to modify their approach to daily activities:
- Prioritize essential tasks during high-energy periods
- Build rest periods into daily schedules
- Recognize personal energy patterns and plan accordingly
- Avoid overcommitment to reduce stress
Regular Medical Care
Maintaining relationships with healthcare providers ensures optimal management:
- Regular endocrinology follow-up every 6-12 months
- Prompt attention to new symptoms or concerns
- Coordination between different specialists
- Staying current with vaccinations to prevent infections
Prognosis and Complications
With proper diagnosis and treatment, most patients with adrenal insufficiency can expect to live normal, productive lives. However, understanding the potential complications and long-term outlook helps patients and healthcare providers work together to optimize outcomes.
Life Expectancy and Quality of Life
Modern hormone replacement therapy has dramatically improved the prognosis for adrenal insufficiency. Most patients achieve near-normal life expectancy when they receive appropriate treatment and follow proper management protocols.
However, some studies suggest a slightly increased mortality risk compared to the general population. This increased risk primarily stems from:
- Adrenal crises during severe illness or inadequate stress dosing
- Increased susceptibility to infections
- Cardiovascular complications related to both the condition and its treatment
- Complications from other associated autoimmune disorders
Quality of Life Factors
Many patients report excellent quality of life with proper treatment, though some experience ongoing challenges:
- Persistent fatigue despite optimal hormone replacement
- Anxiety about potential crises
- Limitations on spontaneous activities due to medication requirements
- Impact on career choices or advancement opportunities
Potential Complications
Adrenal Crisis
Despite proper education and treatment, adrenal crises remain the most serious complication. Statistics show that a small number of patients experience an adrenal crisis annually.
Risk factors for adrenal crisis include:
- Concurrent infections, particularly gastrointestinal illnesses
- Surgical procedures without appropriate stress-dose coverage
- Medication non-adherence or inability to take oral medications
- Lack of patient education about stress dosing
- Delayed recognition of symptoms
Bone Health Issues
Long-term glucocorticoid replacement, especially when doses are higher than physiologic levels, can lead to:
- Osteoporosis and increased fracture risk
- Osteonecrosis, particularly of the hip and shoulder
- Growth retardation in children
Regular bone density monitoring and preventive measures, such as calcium and vitamin D supplementation, help minimize these risks.
Cardiovascular Complications
Both under-treatment and over-treatment can affect cardiovascular health:
- Under-replacement may cause persistent low blood pressure and poor exercise tolerance
- Over-replacement can contribute to hypertension, diabetes, and heart disease
- Optimal dosing requires careful balance and regular monitoring
Metabolic Effects
Improper hormone replacement can lead to:
- Blood sugar abnormalities, including diabetes risk with over-replacement
- Weight gain or difficulty maintaining a healthy weight
- Electrolyte imbalances affecting kidney function
Pregnancy and Fertility Considerations

Women with adrenal insufficiency can have successful pregnancies with proper management:
Preconception Planning
- Optimize hormone replacement before conception
- Ensure adequate folic acid supplementation
- Review medications for pregnancy safety
- Establish care with high-risk obstetrics specialists
Pregnancy Management
- Increased glucocorticoid requirements, especially in the third trimester
- More frequent monitoring of hormone levels and clinical status
- Preparation for labor and delivery with stress-dose protocols
- Coordination between endocrinology and obstetrics teams
Fertility Issues
Both men and women may experience fertility challenges:
- Women may have irregular menstrual cycles affecting ovulation
- Men may have reduced testosterone levels and sperm quality
- Proper hormone replacement often improves fertility outcomes
Long-term Monitoring Requirements
Lifelong medical surveillance helps prevent complications and optimize treatment:
Regular Assessments
- Endocrinology visits every 6-12 months minimum
- More frequent visits during medication adjustments or health changes
- Annual comprehensive health evaluations
- Periodic specialist consultations as needed
Screening for Associated Conditions
Patients with autoimmune adrenal insufficiency require screening for other autoimmune disorders:
- Annual thyroid function testing
- Periodic screening for diabetes
- Monitoring for other endocrine abnormalities
- Assessment for celiac disease and other autoimmune conditions
Prevention and Awareness
While many causes of adrenal insufficiency cannot be prevented, understanding risk factors and implementing appropriate preventive measures can significantly reduce the incidence of both the condition itself and its most serious complications.
Preventing Iatrogenic Adrenal Insufficiency
The most preventable form of adrenal insufficiency results from inappropriate management of glucocorticoid treatment. Healthcare providers and patients can work together to minimize this risk:
Proper Steroid Tapering
When patients require long-term steroid therapy for conditions like asthma, rheumatoid arthritis, or inflammatory bowel disease, careful withdrawal protocols prevent suppression of the natural hormone production system:
- Gradual dose reduction over weeks to months, depending on treatment duration
- Monitoring for symptoms of adrenal insufficiency during tapering
- Education about signs that might indicate too-rapid withdrawal
- Consideration of alternate-day dosing to reduce suppression risk
Patient Education for Steroid Users
Patients receiving chronic glucocorticoid treatment should understand:
- The importance of not stopping medications abruptly
- Recognition of adrenal insufficiency symptoms
- When to contact healthcare providers during illness
- The need for stress-dose adjustments during surgery or severe illness
Early Recognition and Diagnosis

Improving awareness among healthcare providers and the general public can lead to earlier diagnosis and better outcomes:
Healthcare Provider Education
Medical professionals should maintain awareness of adrenal insufficiency, particularly:
- Emergency department staff who might encounter an adrenal crisis
- Primary care providers who see nonspecific symptoms like fatigue and weight loss
- Specialists who treat conditions associated with autoimmune disorders
- Surgical teams that need to provide appropriate perioperative steroid coverage
Public Awareness Initiatives
Patient advocacy organizations and medical societies work to increase public understanding:
- Educational campaigns about autoimmune disorders
- Information about when to seek medical evaluation for persistent symptoms
- Resources for newly diagnosed patients and families
- Support networks for ongoing management
Family Screening Recommendations
Genetic Counseling
Families affected by genetic forms of adrenal insufficiency may benefit from:
- Genetic testing to identify carriers of disease-causing mutations
- Family planning counseling for reproductive decisions
- Early screening of at-risk family members
- Education about inheritance patterns and risks
Autoimmune Disease Surveillance
Family members of patients with autoimmune Addison’s disease have an increased risk for other autoimmune conditions:
- Periodic screening for thyroid disorders, diabetes, and other endocrine conditions
- Awareness of symptoms that might suggest autoimmune disease development
- Genetic testing for predisposing factors when appropriate
Emergency Preparedness Education
Community Training Programs
Some communities develop specialized training programs for:
- School personnel caring for children with adrenal insufficiency
- Workplace first aid responders
- Emergency medical services personnel
- Family members and caregivers
Medical Alert Systems
Encouraging widespread use of medical identification helps ensure appropriate emergency care:
- Medical alert bracelets or necklaces with clear condition identification
- Smartphone medical ID features with emergency information
- Wallet cards with medication lists and emergency contacts
- GPS-enabled medical alert devices for high-risk patients
Research and Future Developments
Ongoing research efforts aim to improve prevention and treatment options:
Improved Hormone Replacement
- Development of longer-acting formulations requiring less frequent dosing
- Modified-release preparations that better mimic natural hormone rhythms
- Implantable devices for continuous hormone delivery
- Gene therapy approaches for some genetic forms
Better Diagnostic Tools
- More sensitive tests for early detection of adrenal dysfunction
- Improved methods for distinguishing between different types of adrenal insufficiency
- Point-of-care testing for emergency diagnosis
- Biomarkers for predicting crisis risk
Prevention Strategies
- Research into preventing autoimmune destruction of adrenal glands
- Better understanding of genetic risk factors
- Improved protocols for steroid withdrawal
- Development of protective therapies during high-risk periods
The National Institutes of Health and other research organizations continue to fund studies aimed at improving outcomes for patients with adrenal insufficiency. These efforts focus on both preventing the condition when possible and optimizing treatment for those already affected.
Understanding adrenal insufficiency requires recognition of its complexity, potential severity, and the critical importance of proper medical management. While this rare condition presents significant challenges, patients who receive appropriate treatment and education can expect to live whole, productive lives. The key lies in early recognition, prompt treatment, comprehensive patient education, and ongoing medical support to prevent the most serious complications.
Disclaimer: The information provided by Foot Palace on yourfootpalace.com is provided for educational and informational purposes only and does not constitute providing medical advice. The information provided should not be used for diagnosing or treating a health problem or disease, and those seeking personal medical advice should consult with a licensed physician. Always seek the advice of your doctor or other qualified health provider regarding a medical condition.
(706) 521-5290